What is pain?
Pain is defined by the International Association for the Study of Pain as an “unpleasant sensory and emotional experience with tissue damage or potential tissue damage”. Pain has been recognised as the 6th vital sign (along with blood pressure, heart rate, respiratory rate, oxygen saturation and temperature). This occurs after an injury such as a cut or surgical operation. Pain is perceived differently; therefore the intensity of pain after surgery is subjective to the individual pain threshold. This also includes the patient’s mental state or condition. Psychologically, pain may lead to anxiety, mood and sleep disturbance.
What types of pain are there?
There are two types of pain;
Acute Pain occurs immediately after an injury such as trauma or surgery or with a disease e.g. cancer, arthritis, rheumatic disease flare up. This can last from days or weeks up to 3 months
Chronic Pain is pain that lasts longer than 3 or 6 months. This may also develop after an operation known as chronic post-surgical pain e.g. scar pain after an operation.
Acute pain can be a useful protective mechanism when for example; a hand is withdrawn after a painful injury, such as a burn. On the contrary, chronic pain is not protective and may affect mobility, physical function and the quality of life in general.
Pain while in hospital
Both acute and chronic pain can occur while in hospital. Nowadays pain is diagnosed and treated earlier however sometimes it can be under-recognised, under-estimated or under-treated while staying in hospital. Therefore it is important to know that patients need to ask for pain killers if they experience any type of pain especially if pain is moderate to severe.
Pain assessment
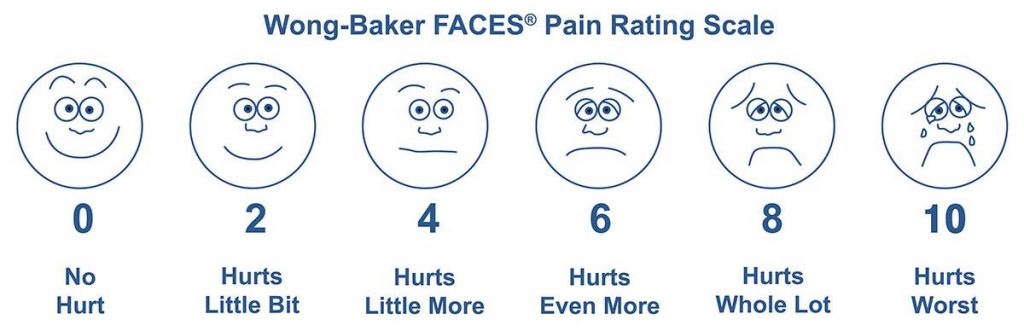
Pain can be assessed using various scores such as the visual analogue scale (a scale of zero to ten, ten being maximum pain and zero is no pain at all) or the Wong Baker faces (see below).
Different modes of pain treatment
- Oral tablets or liquid
- Can be taken before and after the operation.
- Patients need to be able to eat and drink (not suitable if you are sick or vomiting).
- Usually take about 30 minutes to work.
- May not be sufficient to control severe pain.
- Suppositories
- Given before, during or after the operation.
- Useful if the patient is sick, cannot swallow or cannot eat.
- Injections
- Can be administered before, during or after the operation.
- It is administered intravenously (into the vein), intramuscular (into a muscle- usually buttock, thigh or arm) or subcutaneously (just under the skin).
- Anti-sickness, anti-itching and anti-inflammatory medications amongst others can be given via this route.
- PCA- Patient controlled analgesia
- Given after the operation.
- A pump is attached to Patient’s drip and the patient can administer a small bolus of a strong pain killer e.g. morphine, by pressing a button.
- It is safe and should only be used by patient.
- A lockout period is present to between boluses to prevent overdosing.
- Local anaesthetic infiltration
- Administered during the operation, usually by the surgeon on and around the wound.
- This may reduce pain for several hours after the operation.
- Spinal/Epidural
- This is sited before the operation.
- Spinal anaesthesia is a single injection into the lower back to numb the lower part of the body as a single anesthetic or in combination with a general anaesthetic.
- An epidural is a small plastic catheter inserted into the lower back, usually done for larger operations e.g. laparotomy, gastrectomy. This may be removed at the end of operation or stay in place for pain relief for a few days.
- Peripheral nerve blocks
- Administered before, during or after the operation.
- Involves injection of local anaesthetic around a nerve or nerve bundle by the anaesthetist with or without the use of ultrasound.
- Provides a good pain relief for hours after the operation and it can also be used as a sole anaesthetic.
Treatment of acute pain
Prevention, early diagnosis and effective treatment has shown to reduce the risk of developing chronic pain. Pain is treated or prevented with different pain killers. It is usually treated with regular basic pain killers (e.g. Paracetamol and ibuprofen) with or without the combination of stronger medications e.g. Codeine, Tramadol and Morphine
These medications can be given as tablets, liquids, suppositories, injections into a vein or muscle, local anaesthetic infiltration, spinal or epidural anaesthesia and peripheral nerve blocks.
Treatment of chronic pain
The treatment of chronic pain includes various aspects and modalities (multi-modal approach) and often involves different healthcare professionals (multi-disciplinary approach).
More complex patients are often given an appointment in the pain clinic where they are usually reviewed by a pain consultant. Rheumatologists, physiotherapists, neurologists, psychologists and psychiatrists are also seeing chronic pain patients in the out-patients department. A referral by the GP is necessary.
Available treatment options at the Pain Clinic are:
- Education, Information and Reassurance and general advice (activity pattern, awareness, mindfulness to avoid inactivity and painful flare ups)
- Regular exercising and stretching to maintain and improve range of movement, mobility and symptom progression and subsequently quality of life (This includes core exercises, non-impact exercises, such as swimming, cycling, walking, Yoga, Pilates, Tai-Chi)
- Physiotherapy for specific exercises and physical therapy (including hydrotherapy, massage, acupuncture as applicable)
- Operations (for some patients an operation may be considered after consultation with a surgeon, e.g. hip or knee replacement, treatment of endometriosis, median or ulnar nerve release, lumbar or cervical fusion or discectomy or decompression)
- Medication (Paracetamol, Anti-inflammatories, weak and strong opioids, Anti-neuropathic medications such as antidepressants and antiepileptics, topical treatments such as numbing patches)
- Injections around the spine with X-ray or around peripheral nerves under ultrasound guidance. Injections will not solve a long-term pain condition, but they may provide more than 50% pain relief for up to 6-12 months. The primary principle is not to harm patients. Therefore, a less invasive injection therapy may be tried first. Examples of injections are: facet joint injections, sacroiliac joint injections, radiofrequency-denervation, pulsed radiofrequency, Dorsal Root Ganglion., Nerve root blocks, Epidurals, Peripheral nerve blocks; Greater occipital nerve, , Genitofemoral nerve, Genicular branches, Stellate ganglion, coeliac plexus, Blocks; Bier‘s blocks, Trigeminal Nerve Blocks, RACS-catheters, Spinal Cord Stimulators (SCS) and more . The Pain Doctor will guide you to what intervention is suitable for each individual case.
- Complimentary treatments TENS-machine, Acupuncture, Chiropracter, Osteopath)
- Psychological and counselling – psychological help offered with regards to pain management as in or out patient
- Referral to other specialists (e.g. for a scan, Neurologist, Rheumatologist, Surgeon, Physiotherapist).
- Follow up appointments or re-referral if needed
Referral to the pain clinic
- Difficulties in managing chronic pain (in particular complex pain patients with many co-existing diseases, multiple different medications, kidney and liver failure)
- Need of non-pharmacological treatments, Medication not effective
- Risk of long-term distress, disabling pain
- Complex Cancer Pain
- Refractory abdominal, renal and post-surgical pain
- Resistant trigeminal neuralgia and postherpetic neuralgia
- Complex Regional Pain syndrome
- Others
For urgent referrals it is best to speak directly to a Pain Consultant.
Information needed in the pain clinic – Questions you may be asked
- How long for? When did it start? Sudden or gradual onset?
- Is pain constant or intermittent? Periodic / Episodic worsening, how often?
- Intensity (on a good day and on a bad day: 0-10 / 10)
- Where do you feel the worst pain? – Is pain going or radiating anywhere else?
- How does pain feel? (dull, aching, sharp, shooting, like an electric shock, stabbing, throbbing, prickling, tingling, numb)
- What makes pain worse? (e.g. certain activities, walking, lifting, standing, sitting, driving, coughing, sneezing)
- What makes pain better, what helps? (e.g. medication, rest, hot water bottle)
- What does pain stop you from doing?
Associated symptoms
- Are mood and sleep affected
- Do you feel anxious, angry or depressed
- Inactivity / Loss of mobility?
- Red flag symptoms (e.g. bladder or bowel problems, recent falls, infections or fractures, unexpected weight loss, new weakness or numbness in the leg or arm)
Current medication
- Pain medication now and in the past (for how long, side effects, tolerability)
- Is the pain medication (and each of it) effective
- Disease-modifying drugs (anti-rheumatics)
- Any chemotherapy or radiotherapy in the past?
- Other medication (blood pressure, heart, breathing, gout, anti-rheumatic drugs)
- Allergies
Past medical history
- cardiovascular (Blood pressure, heart attacks, stroke, Blood clots in veins or lungs)
- Respiratory (COPD, asthma)
- Diabetes
- Liver and Kidney failure
- Rheumatic diseases, Osteoporosis
- Heartburn, Reflux disease
Social History
- Partner, children, friends
- Employment (part-time, full-time)
- Driving
- Sport, Hobbies
- Sleep, Mood
Previous scans
- X-rays
- Ultrasounds
- Images
Previous Treatments
- Physiotherapy, Hydrotherapy, Massage, Exercise classes
- Injections (when, what, by whom?)
- Acupuncture, TENS
- Hot, cold applications
- Chiropractor, Osteopaths
What are your expectations?
- more effective medication, other medication, medication reduction
- injections
- general advice about activity and pain reduction
- referral to other specialist





